
Short answer: Yes!
In recent decades, sauna bathing has emerged as a means to increase lifespan and improve overall health, based on compelling data from observational, interventional, and mechanistic studies. Of particular interest are the findings from studies of participants in the Kuopio Ischemic Heart Disease Risk Factor (KIHD) Study, an ongoing prospective population-based cohort study of health outcomes in more than 2,300 middle-aged men from eastern Finland, which identified strong links between sauna use and reduced death and disease.
How much should I Sauna?
Short answer: As much as possible!
The KIHD findings showed that men who used the sauna two to three times per week were 27 percent less likely to die from cardiovascular-related causes than men who didn’t use the sauna. Furthermore, the benefits they experienced were found to be dose-dependent: Men who used the sauna roughly twice as often, about four to seven times per week, experienced roughly twice the benefits – and were 50 percent less likely to die from cardiovascular-related causes.[2] In addition, frequent sauna users were found to be 40 percent less likely to die from all causes of premature death. These findings held true even when considering age, activity levels, and lifestyle factors that might have influenced the men’s health.
The KIHD also revealed that frequent sauna use reduced the risk of developing dementia and Alzheimer’s disease in a dose-dependent manner. Men who used the sauna four to seven times per week had a 66 percent lower risk of developing dementia and a 65 percent lower risk of developing Alzheimer’s disease, compared to men who used the sauna only one time per week.
The health benefits associated with sauna use extended to other aspects of mental health, as well. Men participating in the KIHD study who used the sauna four to seven times per week were 77 percent less likely to develop psychotic disorders, regardless of the men’s dietary habits, socioeconomic status, physical activity, and inflammatory status (as measured by C-reactive protein).
How does it work? whats the mechanisims?
Physiological response to heat stress
Exposure to high temperature stresses the body, eliciting a rapid, robust response. The skin and core body temperatures increase markedly, and sweating ensues. The skin heats first, rising to 40°C (104°F), and then changes in core body temperature occur, rising slowly from 37°C (98.6°F, or normal) to 38°C (100.4°F) and then rapidly increasing to 39°C (102.2°F).
Cardiac output
a measure of the amount of work the heart performs in response to the body’s need for
oxygen, increases by 60 to 70 percent, while the heart rate (the number of beats per minute) increases and the stroke volume (the amount of blood pumped) remains unchanged. During this time, approximately 50 to 70 percent of the body’s blood flow is redistributed from the core to the skin to facilitate sweating. The average person loses approximately 0.5 kg of sweat while sauna bathing. Acute heat exposure also induces a transient increase in overall plasma volume to mitigate the decrease in core blood volume. This increase in plasma volume not only provides a reserve source of fluid for sweating, but it also acts like the water in a car’s radiator, cooling the body to prevent rapid increases in core body temperature and promoting heat tolerance.
Stresses the body which activate beneficial responses.
Repeated sauna use acclimates the body to heat and optimizes the body’s response to future exposures, likely due to a biological phenomenon known as hormesis, a compensatory defense response following exposure to a mild stressor that is disproportionate to the magnitude of the stressor. Hormesis triggers a vast array of protective mechanisms that not only repair cell damage but also provide protection from subsequent exposures to more devastating stressors.
The physiological responses to sauna use are remarkably similar to those experienced during moderate- to vigorous-intensity exercise. In fact, sauna use has been proposed as an alternative to exercise for people who are unable to engage in physical activity due to chronic disease or physical limitations.
Molecular mechanisms involved in the heat stress response
The hormetic effects of heat stress are facilitated by molecular mechanisms that mitigate protein damage and aggregation and activate endogenous antioxidant, repair, and degradation processes. Many of these responses are also triggered in response to moderate- to vigorous-intensity exercise and include increased expression of heat shock proteins, transcriptional regulators, and pro- and anti-inflammatory factors.
Heat shock protein activation
Baseline level of heat shock proteins depends on the amount of overall heat acclimation.
Heat-shock proteins (HSPs) comprise a large, highly conserved family of proteins that are present in all cells. They play prominent roles in many cellular processes, including immune function, cell signaling, and
cell-cycle regulation.
Under normal conditions, cells maintain a constant, or “basal,” level of HSPs to facilitate several aspects of the protein synthesis machinery, including assembly, folding, export, turn-over, and regulation. However, normal metabolic processes and immune function create reactive byproducts (such as reactive oxygen species and reactive nitrogen species) that can damage proteins and disrupt their structure. Intrinsically disordered proteins are common features in cardiovascular diseases, and damaged, dysfunctional proteins, which can aggregate, or clump together, are strongly implicated in the pathogenesis of neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease, and Huntington’s disease. Increased expression of HSPs prevents protein disorder and aggregation by repairing proteins that have been damaged, and, in fact, animal evidence suggests that HSPs may offer protection against neurodegenerative diseases.
When cells are stressed due to changes in their environment, cellular proteins can unfold or become damaged, impairing their normal function and further increasing their vulnerability to change. During exposure to stress from temperature extremes, reduced nutrient levels (as in fasting), or hypoxia (reduced oxygen), cells increase expression of HSPs to stabilize unfolded proteins and repair or re-synthesize damaged ones. This phenomenon, referred to as the heat shock response, occurs at the expense of other cellular proteins to protect the cell from damage.
Heat stress, in particular, robustly activates the heat shock response. For example, after healthy men and women sat in a heat stress chamber for 30 minutes at 73°C (163°F), their levels of HSP72 increased by 49 percent.[21] In a different study, in which healthy men and women were exposed to deep tissue heat therapy for six days, participants’ levels of HSP70 and HSP90 increased 45 percent and 38 percent, respectively.[22] In addition, their biomarkers of mitochondrial biogenesis improved, and their mitochondrial function increased by 28 percent compared to baseline levels. This activation of HSPs is sustained over time, suggesting that heat acclimation induces whole-body adaptations that increase heat tolerance, resulting in protective cellular adaptations.
Sauna activates longivity protiens / Genes / and pathways
NRF2
The HSP70 family of proteins is the most abundant of all the HSPs. Data from a longitudinal study of Danish nonagenarians showed that genetic variants of HSP70 influenced lifespan in females, with carriers of one haplotype living approximately one year longer than non-carriers.
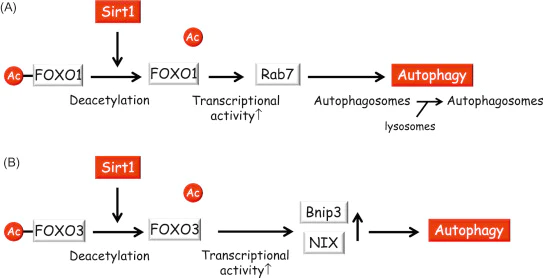
FOXO3
FOXO3 proteins are members of the FOX family of highly conserved transcriptional regulators. They play important roles in human lifespan and healthy aging. FOXO3s regulate a vast number of genes that combat elements of cellular aging, such as damage to DNA, proteins, and lipids, and loss of stem cell function. They also increase the production of genes that regulate DNA repair, tumor suppression, stem cell function, immune function, and protein aggregation to further mediate the deleterious effects of aging. FOXO3s participate in autophagy, but when autophagic mechanisms are disturbed, FOXO3s confer cellular sensitization to apoptosis, a type of programmed cell death.
Following heat stress, FOXO3 proteins form a complex with sirtuin 1, or SIRT1, an enzyme that influences aging and longevity via multiple molecular pathways. Sirtuins regulate a variety of metabolic processes,
including release of insulin, mobilization of lipids, response to stress, and modulation of lifespan. SIRT1
enhances FOXO3’s resistance to oxidative stress and its ability to induce cell cycle arrest, but it also inhibits FOXO3’s ability to induce apoptosis, shifting FOXO3 activities away from cell death and toward stress resistance.
Health benefits associated with sauna use
Cardiovascular health
Heat exposure induces protective responses against the deleterious biological processes that drive cardiovascular disease and related disability. Some of these responses recapitulate those experienced during exercise. For example, heart rate may increase up to 100 beats per minute during moderate-temperature sauna bathing sessions and up to 150 beats per minute during hotter sessions, similar to the increases observed during moderate- to vigorous-intensity physical exercise.[36][37] Furthermore, in a study involving 19 healthy adults, the effects of a single 25-minute sauna session were comparable to moderate physical exercise with respect to cardiovascular measures. During sauna use or moderate exercise, the participants’ heart rate and blood pressure increased immediately, but after the sauna or exercise session, participants’ blood pressure and heart rate began to drop below baseline levels measured pre-sauna or -exercise.[38] Like exercise, long-term sauna use generally improves blood pressure, endothelial function, and left ventricular function, and reduces inflammation.
Cardiovascular disease
The World Health Organization estimates that nearly 18 million people die each year from cardiovascular diseases, roughly one-third of all deaths worldwide. Cardiovascular disease is largely preventable with lifestyle behaviors such as sauna use. As described above, large prospective studies conducted in eastern Finland have shown that compared to men who only used the sauna once per week, moderate sauna users (2-3 times per week) are 22% less likely to experience sudden cardiac death, and frequent users (4-7 times per week) are 63% less likely to experience sudden cardiac death.[2] In addition, the frequent sauna users were found to be 37 percent less likely to die from all causes of premature death, regardless of age, activity levels, and lifestyle factors.
Congestive heart failure
Congestive heart failure, or CHF, represents the culmination of all forms of cardiovascular disease. It leads to impaired blood flow to the heart and peripheral tissues with subsequent functional losses, shortness of breath, fluid retention, and left ventricular hypertrophy. Treatment is often limited to pharmaceutical, dietary, or palliative care.
Findings from a prospective, multicentered, randomized controlled trial involving 149 patients with
advanced CHF demonstrated that two weeks of waon therapy improved the patients’ endurance, heart size, and disease status compared to those who received standard medical care.[39] In a different randomized controlled trial involving 30 CHF patients with frequent premature ventricular contractions, or PVCs, a type of abnormal heartbeat, researchers found that two weeks of infrared dry sauna (waon therapy) reduced the number of PVCs the patients experienced in a 24-hour period (from a baseline of ~3161 to ~848). A control group that received conventional medical therapy showed no changes.
Ischemic heart disease
Ischemic heart disease, also known as coronary artery disease, is characterized by reduced blood supply to the heart. It is the most common cause of death in most western countries. A randomized controlled
trial examined the effects of sauna use in 24 patients with ischemic heart disease with chronic total coronary artery occlusion (full blockage of one or more of the arteries that supply the heart) who had not responded to non-surgical procedures and were not candidates for surgical interventions. The findings demonstrated that 15 waon sessions given over a three-week period improved the patients’ vascular endothelial function. No improvements were observed in the control group that received standard medical care.
Peripheral artery disease
Peripheral artery disease, or PAD, is a painful and debilitating condition in which the arteries that supply the head and extremities narrow. A pilot trial involving 20 patients with PAD who received 50 waon sessions over a period of 10 weeks demonstrated improvements in pain levels, walking endurance, and lower extremity blood flow.[42] A similar randomized controlled trial involving 21 patients with PAD showed comparable improvements.
Dyslipidemia
Dyslipidemia, or abnormal blood lipid levels, is a strong predictor of cardiovascular disease risk. Two small studies have shown that regular sauna use modulates serum cholesterol and lipoproteins in healthy adults. Women who were exposed to seven 30-minute sauna baths over a period of two weeks exhibited reduced total cholesterol levels (from ~4.47mmol/L to ~4.25mmol/L) and reduced low-density lipoprotein, or LDL, levels (from ~2.83mmol/L to ~2.69mmol/L).[44] Similarly, men who were exposed to ten 45-minute sauna baths over a period of three weeks exhibited reduced total cholesterol levels (from ~4.50mmol/L to ~4.18mmol/L) and reduced LDL levels (from ~2.71mmol/L to ~2.43mmol/L).
Hypertension
Hypertension, defined as a systolic pressure of 130 mm Hg or higher, or a diastolic pressure of 80 mm Hg or higher, is a chronic elevation of blood pressure.[46] It is a robust predictor of future incidence of stroke, coronary heart disease, heart attack, heart failure, and cardiovascular-related death. Central to the
pathophysiology of hypertension is the loss of arterial compliance, or elasticity, which can have
far-reaching effects on multiple organ systems, including the brain and kidneys. A common element among sauna users, however, is lower incidence of hypertension through improvements in arterial compliance. For example, men who used the sauna two to three sessions every week were found to have a 24 percent lower risk of developing hypertension, and men who used the sauna four to seven times per week had a 46 percent lower risk for hypertension, compared to men who used the sauna only once per week. Just a single sauna session has been shown to lower blood pressure and improve arterial compliance. As such, sauna use may serve as a non-pharmacological means to address, or even prevent, hypertension.
Endothelial dysfunction
The endothelium, the cell layer that lines the blood vessels, secretes substances that regulate blood vessel
dilation (vasodilators) and constriction (vasoconstrictors). Endothelial dysfunction is characterized by decreased secretion of vasodilators and/or increased secretion of vasoconstrictors. This imbalance leads to impaired endothelium-dependent vasodilation, which is common among people who have CHF. Two weeks of sauna therapy, however, improved endothelial and cardiac function in patients with CHF.
Left ventricular dysfunction
Dysfunction of the heart’s left ventricle sets in motion a cascade of compensatory mechanisms that promote organ-level structural changes and elicit system-level hormonal adaptations. It is widely recognized as the end-stage of heart failure. Both single-session and long-term (five days per week for four weeks) sauna use improved ventricular function in men with CHF and may have therapeutic value for treating late-stage cardiovascular disease.
Inflammation
Inflammation is a critical element of the body’s immune response that involves immune cells, cell-signaling proteins, and pro-inflammatory factors. Acute inflammation occurs after minor injuries or infections and is characterized by local redness, swelling, or fever. Chronic inflammation occurs on the cellular level in response to toxins or other stressors and is often “invisible.” It plays a key role in the development of many chronic diseases, including cancer, cardiovascular disease, and diabetes.
C-reactive protein, or CRP, one of several blood proteins often referred to as acute phase reactants,
participates in the body’s inflammatory cascade. Elevated CRP is associated with the development of
atherosclerosis, loss of arterial compliance, and incidence of cardiovascular events. Sauna use, however, reduces blood levels of CRP. In a study of more than 2,000 men living in Finland, CRP levels were inversely related to the frequency of sauna bathing in a dose-response fashion, with lower levels linked to greater
frequency.
As described above, IL-10 is a potent endogenous anti-inflammatory protein. In a study involving 22 healthy male athletes and non-athletes who received two 15-minute sauna sessions at 98.2°C (208°F) separated by a 5-minute cool shower, the men’s resting IL-10 levels increased, and this adaptation occurred faster in the athletes. A slight increase in some of the HSPs was also observed.
Cognitive & mental health
Enhanced neurogenesis. Heat stress and exercise increase the expression of brain-derived neurotrophic factor, or BDNF, a protein that acts on neurons in the central and peripheral nervous systems, to promote the growth of new neurons. BDNF modulates neuronal plasticity and ameliorates anxiety and depression from early-life stressful events. It is active in the hippocampus, cortex, cerebellum, and basal forebrain – areas involved in learning, long term memory, and executive function. BDNF is also produced in exercising muscle tissue, where it plays a role in muscle repair and the growth of new muscle cells.
Cognitive decline
Normal cognitive function relies on sufficient blood flow to the brain and peripheral nervous system, so cardiovascular diseases and cognitive decline often go hand-in-hand. For example, hypertension alters the structure of cerebral blood vessels and impairs blood flow to the brain. Poor cerebral blood flow is commonly observed in mice and humans and may contribute to impaired amyloid-beta clearance, thereby accelerating the progression of Alzheimer’s disease. In addition, heat exposure increases the production of BDNF to promote neurogenesis – the growth of new neurons in the brain (as described above). Findings from a large observational study of middle-aged men living in Finland demonstrated that men who used the sauna four to seven times per week had a 65 percent reduced risk of developing Alzheimer’s disease, compared to men who used the sauna only one time per week.
Depression
Elevated biomarkers of inflammation are commonly observed in people who have depression. Chronic
activation of the body’s inflammatory response system promotes the development of depressive symptoms and induces changes in brain and neuroendocrine function. Sauna use has been shown to reduce symptoms of depression.
In a randomized controlled trial involving 28 people diagnosed with mild depression, participants who
received four weeks of sauna sessions experienced reduced symptoms of depression – such as improved
appetite and reduced body aches and anxiety – compared to the control group, which received bedrest
instead of sauna therapy.
In a randomized, double-blind study of 30 healthy adults diagnosed with depression, participants who were exposed to a single session of whole-body hyperthermia in which core body temperature was elevated to 38.5°C (101.3°F) experienced an acute antidepressant effect that was apparent within a week of treatment and persisted for six weeks after treatment.
Similarly, in a double-blind randomized controlled trial in which core body temperature was elevated by 1.5°C (2.7°F), IL-6 levels in participants increased markedly, and participants with the highest IL-6 levels had the lowest levels of depression one week later (see discussion with Dr. Charles Raison at 44:18). Some of these benefits may be due to the effects of heat stress on circulating levels of pro-inflammatory IL-6 and the reciprocal effects of IL-10 (as described above).
Beta-endorphins and the opioid system. Another factor that may play a role in mental or cognitive effects from sauna use may depend on the opioid system. Beta-endorphins are endogenous opioids that are part of the body’s natural painkilling system. They are produced and stored primarily in the anterior pituitary gland of the brain and play important roles in pain management and reward circuitry. Evidence suggests that beta-endorphins are responsible in part for the “feel-good” response to exercise.[61] The binding of beta-endorphins to mu-opioid receptors on nerve cells suppresses the release of pain-promoting substances in the brain. Sauna use promotes robust increases in beta-endorphins.
The body also produces an opioid called dynorphin, which is generally responsible for dysphoria, a profound sense of unease or dissatisfaction. Dynorphin also mediates the body’s response to heat, helping the body to cool.[65] Dynorphin is produced in many different parts of the brain, including the hypothalamus, the striatum, the hippocampus, and the spinal cord. The binding of dynorphin to
kappa-opioid receptors triggers cellular events that promote pain and distress.
Sauna use (or intense exercise) promotes dynorphin release, which may be responsible for the general sense of discomfort experienced during heat exposure. Interestingly, in a biological feedback response that occurs after dynorphin binds to the kappa-opioid receptor, the brain produces more mu-opioid receptors, sensitizing them to endorphin and future endorphin exposure.
Mental focus and attention span
Two key players in cognitive and mental function are norepinephrine, a hormone and neurotransmitter produced in the brain, and prolactin, a hormone released by the pituitary gland. Norepinephrine enhances focus and attention, while prolactin promotes myelin growth, which makes the brain function faster, a critical feature in repairing nerve cell damage.
When young men stayed in a sauna that was heated to 80°C (176°F) until subjective exhaustion, their norepinephrine levels increased by 310 percent and their prolactin levels increased by 900 percent. Levels of cortisol, a hormone commonly associated with the stress response, were slightly decreased.[5][69] Similarly, in a study involving women who participated in 20-minute sessions in a dry sauna twice a week experienced a 86 percent increase in norepinephrine and a 510 percent increase in prolactin after the session.
These findings suggest that since the norepinephrine response to exercise is blunted in children with attention deficit hyperactivity disorder, or ADHD, and norepinephrine reuptake inhibitors are frequently
prescribed to treat ADHD, use of heat stress and its acclimation may one day be a useful alternative
therapeutic approach employed by clinicians within some yet-to-be-established age-appropriate protocol.
Hormonal and metabolic function changes with Sauna
Growth hormone
Two 20-minute sauna sessions at 176°F separated by a 30-minute cooling period elevated growth hormone levels two-fold over baseline, and two 15-minute sauna sessions at 212°F dry heat resulted in a five-fold increase in growth hormone.
Insulin and glucose
Insulin regulates glucose homeostasis, primarily by promoting the uptake of glucose into muscle and
adipose tissue. Repeated treatment with a far-infrared sauna has been shown to significantly lower fasting blood glucose levels.[74] When insulin resistant diabetic mice were subjected to 30 minutes of heat treatment three times a week for 12 weeks, they experienced a 31 percent decrease in plasma insulin levels and a significant reduction in blood glucose levels, suggesting re-sensitization to insulin. The heat treatment specifically targeted the skeletal muscle by increasing the expression of a type of transporter known as GLUT 4, which is responsible for transporting glucose into skeletal muscle from the bloodstream. Decreased glucose uptake by skeletal muscle is one of the mechanisms that leads to insulin resistance.
Physical fitness and athletic performance Sauna benefits

Heat stress from using the sauna may modulate improvements in physical fitness and athletic performance by increasing endurance and maintaining or promoting gains in muscle mass.
Increased endurance
One small intervention study looked at the effects of repeat sauna use on athletic performance and other physiological effects in six male distance runners. The findings showed that one 30-minute sauna session twice a week for three weeks post-workout increased the time that it took for the study participants to run until exhaustion by 32 percent compared to their baseline. These performance improvements were accompanied by a 7.1 percent increase in plasma volume and a 3.5 percent increase in red blood cells (RBCs). During exercise, RBCs transport oxygen from the lungs to the body’s tissues (especially working
muscles) and deliver carbon dioxide to the lungs for expiration. Increases in RBC levels may facilitate these processes and improve performance.
Muscle mass maintenance
Muscular atrophy, the shrinking or wasting away of muscle tissue, commonly occurs with muscle immobilization or disuse following sports injuries. Atrophy causes substantial strength losses, especially during the first week of immobilization or disuse, due to reduced protein synthesis and increased protein degradation.
Maintaining muscle mass requires a balance of new protein synthesis and existing protein degradation. While new protein synthesis accompanies muscle use during exercise, protein degradation can occur during both muscle use and disuse. Of critical importance, therefore, is net protein synthesis.
Heat acclimation, which can be achieved through sauna use, may reduce the amount of protein degradation that occurs during disuse by increasing HSPs, reducing oxidative damage, promoting release of growth hormone, and improving insulin sensitivity. Maintaining positive net synthesis has special relevance for recovery from injury since injury can tip the balance towards protein degradation and away from protein synthesis in the muscles, which can promote muscle atrophy.
A small intervention study in humans found that daily heat treatments applied locally to muscle during 10 days of immobilization prevented the loss of mitochondrial function, increased HSP levels, and attenuated skeletal muscle atrophy by 37 percent compared to a sham control group.[89] These results have been replicated in animal studies. For example, when rats received whole body hyperthermia at 41°C (105.8°F) for 30 minutes or 60 minutes, hindlimb muscle atrophy during disuse decreased by 20 percent or 32 percent, respectively.[87][90] In addition, exposing mouse myoblasts, the embryonic precursors of muscle cells, to heat (42°C [106°F] for 30 minutes) enhanced the activity of transcription factors involved in myogenesis, the process of generating skeletal muscle.[91] This may have special relevance for slowing age-related sarcopenia, a progressive condition characterized by loss of skeletal muscle mass and strength. It is a leading cause of functional decline and loss of independence in older adults.
(105.8°F) for seven days induced a robust expression of HSPs (including HSP32, HSP25, and HSP72) in muscle, correlating with 30 percent more muscle regrowth than a control group subsequent to a week of
immobilization.[86] This HSP induction can persist for up to 48 hours after heat shock. Heat
acclimation causes a higher basal expression of HSPs (even when not exercising) and a more robust
induction upon elevation in core body temperature (such as during exercise).
Heat shock proteins, described above, can prevent muscle protein damage by directly scavenging reactive
oxygen species and by supporting cellular antioxidant capacity through their effects on maintaining the
endogenous antioxidant glutathione. In addition, HSPs can repair misfolded, damaged proteins, thereby
ensuring proteins maintain their proper structure and function.
Sauna and Detoxification

Heavy metals
Heavy metals are naturally-occurring metallic elements that are toxic or poisonous at low concentrations.
Exposures to heavy metals in everyday products such as arsenic in agricultural products, cadmium in
cigarette smoke and automobile exhaust, lead in toys, and mercury in dental amalgam and certain types of fish, are common occurrences. Some heavy metals are excreted in sweat, and sauna use may facilitate their
excretion. In a study in which the presence of various compounds (including heavy metals) in the blood, urine, and sweat of 20 adults was measured, markedly higher excretion of aluminum (3.75-fold), cadmium (25-fold), cobalt (7-fold), and lead (17-fold) was observed in sweat versus urine.
Bisphenol A
Bisphenol A, or BPA, is a chemical used during the production of polycarbonate plastics and epoxy resins. It is ubiquitous in the environment and can be found in plastic beverage bottles and food packaging, metal food and beverage can linings, dental composites and resins, and other products. BPA is an endocrine disruptor that can mimic naturally occurring hormones in the body like estrogens, androgens, and thyroid hormones, potentially altering normal hormonal signals. High levels of urinary BPA are associated with increased risk for cardiovascular disease and diabetes.
Bisphenol A bioaccumulates primarily in adipose tissue in humans, but some evidence indicates that it is
excreted via sweat and, to a lesser degree, urine. Sauna bathing may serve as means to facilitate BPA
excretion via the skin to eliminate this toxicant from the human body.
Polychlorinated biphenyls
Polychlorinated biphenyls, or PCBs, are organochlorine compounds historically used in industrial and chemical applications such as coolants, transformer insulators, capacitors, motors, paints, and electrical wire coatings. Although PCBs were banned in the 1970s, they still persist in the environment, and many
freshwater and farmed fish are contaminated with PCBs. Adverse human health effects associated with PCB exposure are related primarily to endocrine disruption, particularly in a developing fetus, as well as increased risk for developing hypertension, cutaneous malignant melanoma, and non-Hodgkin’s lymphoma. PCBs bioaccumulate in human muscle and adipose tissue, brain, liver, and lungs and have long elimination half-lives, ranging from 10 to 15 years. Some, but not all, PCBs are excreted in sweat.
Phthalate compounds
Phthalates are synthetic compounds that are used to create plastic products that are soft and malleable. They are used in other consumer goods including fragrances, paints, nail polish, and food and beverage packaging, and are a ubiquitous component of soft plastic toys as well as various other products, including vinyl floor tiles, shower curtains, synthetic leather, cosmetics, shopping bags, and pharmaceuticals.
Urine samples analyzed from populations worldwide have found phthalates in up to 98 percent of
participants, including pregnant women. Phthalates have a relatively short half-life of less than five hours, which means the widespread detection likely indicates chronic exposure rather than accumulation within the body. Phthalates have been shown to lower testosterone levels and block the effects of testosterone on organs and tissues. Phthalates can pass from mother to fetus through the placenta and may result in abnormal sexual development. Some phthalates but not all are readily excreted through sweat.
Conclusion
Sauna bathing is associated with many health benefits, from cardiovascular and mental health to fertility and athletic endurance. It is generally considered safe for healthy adults and may be safe for special populations with appropriate medical supervision. Heat stress via sauna use elicits hormetic responses driven by molecular mechanisms that protect the body from damage, similar to those elicited by moderate- to vigorous-intensity exercise, and may offer a means to forestall the effects of aging.




